Remdesivir for a few billion more" from Gilead with the European Medicines Agency ?

The European Medicines Agency (EMA) on the grounds of negligence has approved remdesivir as a treatment for Covid-19. A decision potentially has several billion euros on a scientific basis more than questionable if not distorted. The study, pivotal to the recommendation for remdesivir, published in the New England Journal of Medicine is potentially a scientific sham that makes proof readers, the scientific community and ordinary readers unable to find their way in this maze of data and inextricable words.
Besides the overdose of hydroxychloroquine from the British study Recovery would almost be a good student if it had not resulted in probable death from overdose. In addition, after weeks where doctors and researchers have praised the merits of randomized double-blind clinical studies on television, the French government cannot pass up such a sham for a drug that has not proven anything. The French will be satisfied with the Ségur de la Santé, but for Gilead, it will rather be before the film "for a few billion dollars more" that they will drink to the health of Europeans in what can be akin to a "hold- up "in the open. The French will not be fooled.
A short summary as an appetizer before a detailed analysis for those who want to go further.
First of all, this study was to cover 600 "moderate" patients and 400 "severe" patients. Moderate patients receiving three treatments (remdesivir 5 days, remdesivir 10 days and placebo), severe patients receiving two treatments (remdesivir 5 days, remdesivir 10 days).
First, there was a change in the main focus of the study, which is normally prohibited in the protocols. But the beginning of smoking is to realize that in the pre-print that forms the basis of the decision of the European Medicines Agency and the FDA, there is no longer any mention of the duration of treatment at all. The patient inclusion and randomization tree clearly indicates two arms of the study (531 patients receiving remdesivir vs 518 placebo patients) but no longer talks about the two types of moderate versus severe patients. By analysing this inclusion table, we can see that we no longer talk about patients receiving remdesivir for 5 days or 10 days, but the mention appears that in the remdesivir group 180 patients received 10 doses and in the placebo group 185 patients received it. It is therefore no longer possible to look at the patients who received 5 doses or 10 doses in the study or even to identify the health status of the patients on inclusion, and yet Gilead will conclude on these points.
In addition, the study's conclusions, on the reduction in patient hospitalization time, mix "moderate" and "severe" patients. There is so much data missing from the study (nearly 200 patients are excluded for reasons of lack of data, that one can only wonder). A surprising point is the analysis of the mortality on the 14th day of the study as well as the analysis of the initial scores of classification of the patients, because they indicate in the appendix (figure S1) that there were 115 patients in the placebo group with a base score of 7 or 77 with a score of 6 when severe patients were not expected to have placebo. In this study it is therefore impossible to link the text to the tables except in vague places and there is a total inconsistency with the basic objectives.
A detailed analysis of the study results to show the inconsistencies
1. The figure "127 patients" of the favourable curve Plan B
• It is the number of patients that appears in the figures under "no O2" in FIGURE 2 - Plan B which is the most favourable figure for REM (Slide 1)

• 127, this is also the number that appears in Table 1 Group 4 "all" and reported in table S1 Appendix page 22 (Slide 2).

It could therefore be deduced that the 127 patients classified in category 4 of severity is the group of “moderate” patients and that patients classified in groups 1,2 and 3 are the “mild” or mild. Logic would suggest that Gilead considers the 127 patients of category 4 baseline (or the plane B curve here called "oxygen-free") to be "moderate". One of the problems is that the table S1 appendix on page 21 says that the total number of patients in "light and moderate basis" makes 120 patients (Slide 3).

So an offset of 7 patients who disappear.
1. How many patients are there in categories 1,2 and 3 in base? And what is the effect on deaths in the "moderate" patient category. If we take Table 2 below in slide 4, we find a total of 1059 patients (538 and 521). However when we look at categories 4, 5, 6 and 7 we have a total of 1017 people. Unlike the base, we therefore have 42 patients who should be in categories 1, 2 and 3. (Slide 4).

In addition, in slide 2, there are 46 patients in the “unknown” database. But as there are also 46 patients in the “unknown” database !! Looking at slide 4 in category 8 (deaths), in the total group there are 88 people, 33 of whom are from the remdesivir arm and 55 are from the placebo group (in blue). However on these 88 deaths on Day 15 only 2 come from group 4 in base. This group 4 being a priori "moderate", that is to say that we observe: no mortality effect on "a priori moderate" patients. Of the 88 deaths, 24 came from group 5 clearly in favour of remdesivir (4 deaths versus 20), 26 came from group 6 and 33 came from group 7 somewhat favourable to remdesivir (14 deaths versus 19 in the placebo group) The total of group 4, 5, 6 and 7 deaths is 85 deaths. By difference, the number of deaths in groups 1, 2 and 3 is therefore 3 (88 total - 85 groups 4 - 7) Curiously it is on group 5 in base that the numbers are the best for REM. And over the recovery period it is also group 5 which seems to have the best result for the remdesivir treatment; but the study is clear it's just indeed the group scale.
“The benefit was most apparent in patients with a baseline ordinal score of 5 (requiring oxygen), a conclusion most likely due to the larger sample size in this category (since the test d treatment interaction with baseline score on ordinal scale was not significant) " This analysis is found in the fiercepharma article.
1. What table S2 tells us in the appendix
This table shows the two columns with the two arms of the study: Total remdesivir and total placebo.
• Basically, there are 538 patients on remdesivir and 521 patients with placebo for a total of 1059 patients. Complies with table 2.
• Based on this table, there are up to date 15, 844 patients including 434 on remdesivir and 410 on placebo. And the this table gives us an analysis not in relation to the basic group 4, 5, 6 and 7, but in two new groups "light / moderate" and "severe" (Slide 5)

The interest is therefore to compare table 2 and table S2 and to try to understand how Gilead constructed the "light / moderate" group since no explanation is given. The annex S2 table is quite clear: • initially, there are a maximum of 119 "mild and moderate" patients (62 patients on remdesivir and 57 patients on placebo) • on day 15, there are a maximum of 96 “mild and moderate” patients (51 patients on remdesivir and 45 on placebo) • and of the 51 patients treated with remdesivir, 48 found themselves with a score 1,2,3,4 on the 15th day and on the 45 placebo patients, 40 found themselves with a score 1,2,3,4 on the 15th day .
In other words, no benefit of remdesivir compared to placebo on the "mild to moderate" patients in the study. This result is reflected in the last line of this table with the "odd ratio" and the probability "p". For the “light to moderate” group the ratio is 1.13. A ratio close to 1 means that there is no difference. However, the "p values" are absent from the two groups "mild / moderate" and "severe" on the grounds that they did not take the test on the subgroups, while the entire sample had the p-value. is 0.001. This will not fail to attract the attention of our expert. In other words, the rapporteurs give the value "p" for the total sample, but take care not to give it for each of the 2 groups, that is to say that on the "moderate" group, the real result must be hidden.
4. So there remains the double question: where did Gilead get the plan B curve with 127 patients? And, how do we find the probability of a 65% improvement in the condition of patients on day 11 with a 5-day remdesivir treatment for the "light / moderate" group?
Knowing that to distinguish the 5-day and 10-day remdesivir treatment, it is impossible because everything was intentionally mixed. On page 19 of the appendix we find this mention (French translation page 19 appendix): «In the remdesivir arm, 180 participants received 10 doses of remdesivir, 168 patients received <10 doses of remdesivir because they recovered and were discharged from hospital, 21 participants received <10 doses of remdesivir because that they died, 13 participants received <10 doses with missing doses due to a safety or operational problem, and 100 participants were still receiving remdesivir or were missing treatment data on the day of base extraction April 28, 2020 »
In addition, the following elements can be read in various Gilead conclusions:
«The study found that patients in the 5-day remdesivir treatment group were 65% more likely to have clinical improvement on day 11 than those in the standard care group (OR 1.65 [95% CI 1.09 -2.48]; p = 0.017). The odds of improvement in clinical status with 10-day treatment of remdesivir compared to standard of care were also favorable, tending towards but not reaching statistical significance (OR 1.31 [95% CI 0.88- 1.95]; p = 0.18) »
Whereas the study's preprint writes everywhere that there is only remdesivir 10 days.
«Methodology: We conducted a double-blind, randomized, controlled trial with a placebo group and a group treated with intravenous remdesivir in adults hospitalized with Covid-19
with symptoms in the lower respiratory tract. Patients were randomly assigned to receive either remdesivir (200 mg loading dose on day 1, followed by 100 mg daily for up to 9 additional days) or placebo for 10 days »
«Preliminary results from this trial suggest that a 10-day remdesivir treatment was better than placebo. » Incomprehensible.
Here's what Gilead and the study say:
• No statistically significant difference in mortality and clinical deterioration in the placebo group versus the remdesivir group.
• A maximum of 120 patients “light and moderate” inclusive, with a maximum of 96 of these patients were analysed on day 15. • On group 4 on base, a priori closest to “moderate” no mortality on day 15 (in fact 1 death in each group).
• In group 4 as a base, the improvement rate is 90.1% for remdesivir versus 78.4% for placebo, that is to say a ratio of 1.13 not statistically significant (Fig S1 Appendix).
• The study does not make a clear separation between the 10-day and 5-day remdesivir treatment as provided for in the protocol and even less in the results.
• “Moderate” patients treated with remdesivir for 5 days have an improvement ratio of 1.65 with p = 0.017, that is to say approximately 90% improvement for 5-day remdesivir versus 55% for placebo. Where these numbers come from because they are not in the tables anywhere.
• "Moderate" patients with 5-day remdesivir treatment have an insignificant improvement ratio of 1.35.
• Gilead explains that the measurement was made on day 11.
While the study report does not give differentiated results for the 5-day and 10-day treatments and the basic procedure is 10 days, so that remdesivir-5 days and the given day 11 are unknown in the study ! How could such a study, which does not pass the minimum tests of data consistency and concordance, have been the basis for a report by the CHMP (Committee for Medicinal Products for Human Use) and a decision to authorize from the European Medicines Agency? It looks more and more like the famous Mehra study from The Lancet which had to be withdrawn by its authors because they could not prove the origin of the data. We cannot trust the European Medicines Agency, which by its recommendations, built on questionable grounds, publishes a decision which becomes applicable by the member states.
This Agency must be the subject of an in-depth audit which will undoubtedly reveal dysfunctions leading to health risks for Europeans but also serious financial consequences since the State must apply the recommendations not visibly retaining their national sovereignty only on the amount assumed or reimbursed. The sum of few thousand Dollars per treatment in the United States.
It is said that health is priceless, but for a few more euros we would like to see and have convincing results.
À LIRE AUSSI
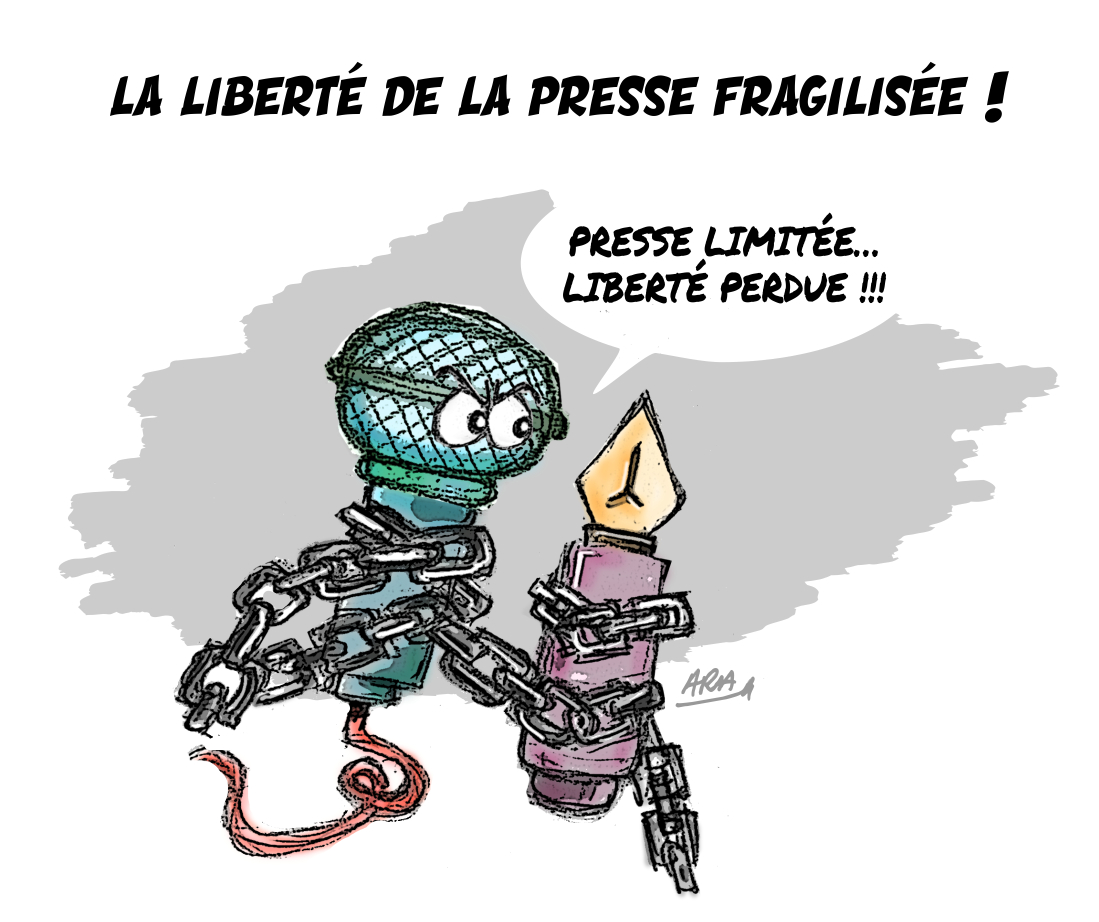
L'article vous a plu ? Il a mobilisé notre rédaction qui ne vit que de vos dons.
L'information a un coût, d'autant plus que la concurrence des rédactions subventionnées impose un surcroît de rigueur et de professionnalisme.
Avec votre soutien, France-Soir continuera à proposer ses articles gratuitement car nous pensons que tout le monde doit avoir accès à une information libre et indépendante pour se forger sa propre opinion.
Vous êtes la condition sine qua non à notre existence, soutenez-nous pour que France-Soir demeure le média français qui fait s’exprimer les plus légitimes.
Si vous le pouvez, soutenez-nous mensuellement, à partir de seulement 1€. Votre impact en faveur d’une presse libre n’en sera que plus fort. Merci.
 Je fais un don
Je fais un don