Covid-19 : is medicine skewed by statistics ?

EDITORIAL: The debate between pro-hydroxychloroquine and those who are against must not turn into a quarrel of churches. Social networks are flourishing with inappropriate, hateful or even defamatory messages between the two "clans". The two groups are scrutinizing the results of the clinical trials in opposite directions. The debate, highly politicized on television, leaving the microphone to doctors who have not had to treat patients or who have links of interest with pharmaceutical companies, gives a poor vision of medicine and medical science.
Observation and empiricism, the fundamental basis of science, are supplanted by the belief that controlled, randomized double-blind clinical trials would provide the highest level of evidence and represent the ultimate scientific approach. A normative “ virtuous method ” free from any defect opposed to “pragmatic empiricism”.
The sponsors of controlled clinical studies would like to make them in a way “hyper sophisticated surveys” where one would ultimately assess through a predefined metric whether there is a positive effect to a treatment. In addition, mathematical processing would be used to measure the statistical efficiency of the metric. So it is not the effectiveness of the treatment that is being measured, but the statistical “effectiveness” of the measurement ! And maybe that's where the perception gap lies.
On the one hand, the "empiricists", "practitioners" of observational medicine (evidence based medicine) evaluate the effectiveness of a treatment on each patient. Following successive observations and keeping in mind that each patient is unique, they try to draw a protocol from the clinical trial. With the advent of controlled trials, patients are uniformly reduced to a collection of 2 dozen clinico-pathological features and are distinguished from each other only by their inclusion number. In a way to to compensate for this dehumanization, let us recall that medical research affirms that it is now moving towards individualized treatments (cf. research on stem cells). Doctors have practiced an individualized adaptation of treatments to patients for a long time. On the other hand, the supporters of the clinical trial (with all its sophistication: randomized, double blinded, controlled…) test one or more treatments and determine if there is a significant difference between them by performing statistical tests.
However, statistical tools are too often misused. In most tests, an attempt is made to measure the power "p" of a result through a statistical test. But this famous "p" is above all a function of the starting hypotheses.
To illustrate this, let's take a simple example : in your car, to compensate for the loss of speed caused by the incline when going uphill, you step on the accelerator. You therefore consider external elements such as slope and friction. The commonly accepted assumption is that you have to accelerate uphill to keep your speed constant. It wouldn't occur to anyone to take their foot off the accelerator to keep the same speed going uphill. By this we mean that the action to be taken on the accelerator is obvious to compensate for the loss of speed.
Theoritically, a clinical trial is set up following several empirical observations that a treatment has an effect on a pathology. The question is whether this treatment is more effective than the drugs already in common use . When prescribing a drug in accordance with the knowledge of medicine at the time, the doctor believes that this treatment will cure. The hypothesis adopted by the doctor is that the treatment has a greater effect than no treatment (placebo effect) and not the opposite.
In clinical trials, the statistical tests used are often a two-sided test because the anticipated effects of new treatments are often marginal. When a drug works spectacularly, there is no need for a trial. As Professor Raoult says, the most significant trial is where a single patient is cured with certainty from an equally certain disease. This is what happened when Pasteur saved Joseph Meister from rabies. N = 1 and the demonstration was made as the certainty of the boy's death was obvious. If little Meister had died, then consideration should have been given to testing on other patients, with less certainty as to the beneficial outcome of the vaccine. Without mentioning this example, Prof. Raoult affirmed this truth, with a barely concealed irony during his parliamentary hearing, attracting sharp criticism from those who had lost sight of this reality .
To test an effect defined a priori as being higher effect (or lower if applicable), a one-sided statistical test is sufficient.
It would not occur to a doctor to test a drug with a known negative effect. All too often in clinical trials, like the one on hydroxychloroquine, a proven antiviral molecule , doctors forget the initial hypothesis and use a bilateral test. They make the mistake of using tests that are somehow "too powerful" with the associated flaw of being too strict in the decision.
In the case of poorly controlled trials in terms of bias, this element opens the door to the error of concluding that a drug is not effective, when it actually is.
The debate between macroeconomists and microeconomists has long been in existence. Recent times give the feeling that the debate is between supporters of individual medicine and medicine of the greatest number, where the interest of the patient as an individual disappears favoring statistics which are easy to interpret one way or the other.. The myth of a single treatment such as a vaccine has never been so strong as medical research officially claims to be moving towards personalized treatments. For a long time, doctors have prescribed through a “prescription” after an individualized diagnosis.
How many times have we seen observations inferred from unverified human laboratory tests in real life situations? How many economic theories observed on population samples have not found their place on a large scale? The Holy Grail of medicine might be to find a single molecule for each disease. But we live in an increasingly individualized world. Whether at Nike or Ford, you can customize your shoe or vehicle, thus generating multiple combinations. So is it reasonable to want to eliminate all viable treatment options (like hydroxychloroquine) to keep only one which would be remdesivir while waiting for a vaccine for a disease that is not fully understood? It would be like asking Nike to make a unique custom shoe for everyone.
In a pandemic, these pseudo-quarrels of scientists, tinged with obvious conflicts of interest, have no place on television shows, as we could agree with both camps, but on different time horizon. With the failure of the large controlled trials (Recovery and Discovery), recent events have just shown that these studies can not be set up and produce reliable results during an epidemic, giving reason to the pragmatic medical approach . My grandmother often told me: "When you grow up, you will change your mind". In a way, for her, I probably didn't have enough experience or perspective to notice my mistakes.
During a crisis, using their expertise, the doctor observes, learns and adjusts his response to patient care as and when. It is the time of a lifetime to have accumulated enough observations to be able to learn a lesson.
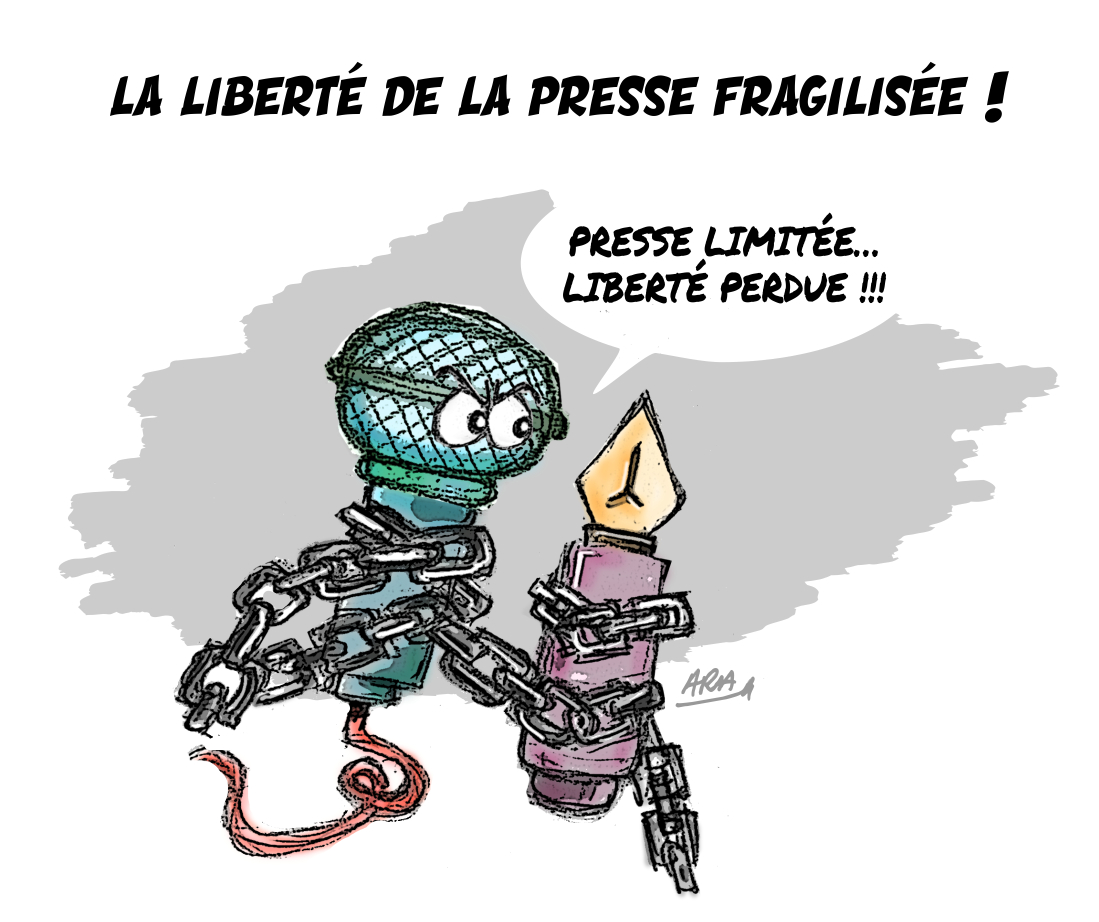
L'article vous a plu ? Il a mobilisé notre rédaction qui ne vit que de vos dons.
L'information a un coût, d'autant plus que la concurrence des rédactions subventionnées impose un surcroît de rigueur et de professionnalisme.
Avec votre soutien, France-Soir continuera à proposer ses articles gratuitement car nous pensons que tout le monde doit avoir accès à une information libre et indépendante pour se forger sa propre opinion.
Vous êtes la condition sine qua non à notre existence, soutenez-nous pour que France-Soir demeure le média français qui fait s’exprimer les plus légitimes.
Si vous le pouvez, soutenez-nous mensuellement, à partir de seulement 1€. Votre impact en faveur d’une presse libre n’en sera que plus fort. Merci.